Recommended Global Nursing Webinars & Conferences
Europe & UK
Asia Pacific & Middle East
Canada
GLOBAL NURSING EDUCATION 2024
- About Conference
- Sessions & Tracks
- Research Excellence Awards
- Become an Exhibitor or Vendor!
- Become a Sponsor!
- Market Analysis
About Conference
The 27th Global Nursing Education, Healthcare and Patient Safety Conference is set to take place on April 25-26, 2024 in Amsterdam, Netherlands. The conference's theme is "Reimagining Nursing Education and Patient Safety for a Resilient Future," which aims to explore innovative ideas and strategies for the advancement of the nursing profession and the enhancement of patient safety.
This conference provides a platform for nursing educators, researchers, practitioners, and students from around the world to share their expertise, experiences, and knowledge. Attendees can expect to participate in interactive discussions, workshops, and poster sessions on a range of topics related to nursing education, healthcare, and patient safety.
Some of the key areas of discussion include the integration of technology in nursing education, the development of leadership skills for nurses, and the implementation of evidence-based practice to improve patient outcomes. Additionally, the conference will highlight the impact of global health challenges, such as the COVID-19 pandemic, on the nursing profession and patient safety.
In addition to the educational sessions, attendees will have the opportunity to network and collaborate with other professionals in the nursing field. This conference will also feature an exhibition area where participants can explore the latest advancements in nursing technology and healthcare products.
Overall, the 27th Global Nursing Education, Healthcare and Patient Safety Conference is a must-attend event for nursing professionals who are interested in advancing their knowledge, skills, and practices. It is an opportunity to learn from experts in the field, share ideas and experiences, and develop new collaborations that will contribute to the resilience of the nursing profession and the safety of patients.
Sessions & Tracks
Session on Innovations in Nursing Education and Curriculum Development
Innovations in nursing education and curriculum development have revolutionized the way aspiring nurses are trained and prepared for their profession. Traditional approaches have given way to dynamic and interactive learning experiences that integrate technology and evidence-based practices. Simulation labs with lifelike patient scenarios allow students to hone their clinical skills in a safe environment, while virtual reality and augmented reality tools enhance their understanding of complex medical procedures. Additionally, online learning platforms provide flexibility and accessibility, enabling nurses to pursue further education while balancing their work and personal commitments. These innovations have transformed nursing education, ensuring that future nurses are equipped with the knowledge and skills needed to deliver high-quality patient care in a rapidly evolving healthcare landscape.
Session on Advancing Technology in Healthcare and Nursing Education
Advancing technology in healthcare and nursing education has transformed the landscape of patient care and learning. Cutting-edge innovations like electronic health records and telemedicine have streamlined communication and improved access to healthcare services. Nurses can now utilize mobile apps and online platforms for continuous learning, accessing educational resources and engaging in collaborative discussions with colleagues worldwide. Virtual reality and simulation technology provide realistic training experiences, allowing nursing students to practice complex procedures in a safe environment. Furthermore, wearable devices and remote monitoring systems enable nurses to monitor patients' vital signs and health conditions remotely, leading to early detection of issues and timely interventions. These advancements in technology have revolutionized healthcare delivery and enhanced nursing education, preparing nurses to adapt to the evolving healthcare industry.
Session on Promoting Cultural Competence in Nursing Education
Promoting cultural competence in nursing education is crucial for providing quality and equitable healthcare. Recognizing the diverse backgrounds and beliefs of patients, nursing programs emphasize the importance of cultural sensitivity and understanding. Through interactive workshops, simulations, and case studies, nursing students learn to navigate cultural differences, develop communication skills, and provide culturally appropriate care. Programs also encourage students to engage with diverse communities through service-learning opportunities, fostering empathy and a deeper understanding of cultural nuances. By integrating cultural competence into the curriculum, nursing education aims to produce culturally sensitive and competent nurses who can deliver respectful, patient-centered care to individuals from various backgrounds, ultimately reducing healthcare disparities and promoting positive health outcomes for all.
Session on Enhancing Interprofessional Collaboration for Patient Safety
Enhancing interprofessional collaboration is crucial for ensuring patient safety and delivering comprehensive healthcare. Recognizing that effective teamwork and communication are essential, healthcare institutions and educational programs emphasize the importance of interprofessional education. Through collaborative learning experiences, such as case studies and simulated scenarios, healthcare professionals from different disciplines learn to work together, share knowledge, and make collective decisions for optimal patient outcomes. Additionally, interdisciplinary team meetings and regular communication channels are established to facilitate information exchange and coordination of care. By fostering a culture of collaboration, healthcare professionals can leverage their unique expertise and perspectives to identify and mitigate potential risks, resulting in improved patient safety, enhanced care quality, and better healthcare outcomes.
Session on Strategies for Nursing Leadership and Management
Effective nursing leadership and management are essential for delivering high-quality patient care and promoting a positive work environment. Successful strategies include fostering open communication and collaboration among team members, promoting a culture of continuous learning and professional development, and creating clear goals and expectations. Nurse leaders prioritize staff empowerment, ensuring that nurses have the necessary resources and support to provide excellent care. They also implement evidence-based practices, monitor performance metrics, and actively seek feedback from both patients and staff. By promoting shared decision-making and creating a culture of accountability, nursing leaders and managers can inspire and motivate their teams, resulting in improved patient outcomes, increased job satisfaction, and a stronger healthcare organization overall.
Session on Integrating Evidence-Based Practice in Nursing Education
Integrating evidence-based practice (EBP) in nursing education is vital for equipping future nurses with the knowledge and skills to provide quality care based on the latest research and best practices. Nursing programs incorporate EBP principles by teaching students how to critically appraise research literature, gather and evaluate evidence, and apply findings to clinical decision-making. Through coursework, clinical experiences, and hands-on projects, students learn to integrate research into their practice, enhancing patient outcomes and healthcare quality. EBP education also fosters a culture of lifelong learning, encouraging nurses to stay updated with the latest evidence and continuously improve their practice. By integrating EBP in nursing education, aspiring nurses become knowledgeable, evidence-driven practitioners who can adapt to changing healthcare landscapes and deliver the best possible care to their patients.
Session on Addressing Health Disparities through Nursing Education
Addressing health disparities through nursing education is essential for promoting equitable healthcare access and outcomes. Nursing programs prioritize teaching students about the social determinants of health and their impact on disparities. By integrating cultural competency training, students learn to provide patient-centered care that respects diverse backgrounds and needs. Nursing curricula also emphasize the importance of community engagement and collaboration with underserved populations. Through clinical rotations and service-learning opportunities, students gain firsthand experience in addressing disparities and advocating for vulnerable populations. By equipping future nurses with the knowledge, skills, and empathy needed to tackle health disparities, nursing education plays a crucial role in creating a more equitable healthcare system for all.
Session on Quality Improvement and Patient Safety Initiatives
Quality improvement and patient safety initiatives are crucial in healthcare to enhance the delivery of safe and effective care. Healthcare organizations implement various strategies to monitor and improve quality, such as implementing evidence-based guidelines, conducting regular audits and assessments, and promoting a culture of open communication and reporting of errors. Patient safety initiatives include measures like medication reconciliation, standardized protocols, and patient engagement in care decisions. Continuous quality improvement involves data analysis, identifying areas for improvement, and implementing evidence-based interventions. By prioritizing quality and safety, healthcare organizations ensure that patients receive the best possible care while minimizing the risk of harm. These initiatives promote a culture of accountability and continuous learning, leading to improved outcomes and patient satisfaction.
Session on Nursing Education for Global Health Challenges
Nursing education for global health challenges prepares nurses to address complex health issues on a global scale. Curricula focus on understanding the social determinants of health, cultural competency, and public health principles. Students learn about global health disparities, infectious diseases, and humanitarian crises, developing skills to assess, plan, and implement interventions. Interdisciplinary collaborations, international field experiences, and cultural immersion programs enhance students' understanding of diverse healthcare systems and global health issues. Emphasis is placed on health promotion, disease prevention, and community engagement. By equipping nurses with a global perspective and the ability to adapt to diverse environments, nursing education prepares future professionals to make a significant impact on global health challenges.
Session on Enhancing Communication Skills in Healthcare Settings
Enhancing communication skills in healthcare settings is vital for effective patient care and positive outcomes. Healthcare professionals are trained to develop active listening skills, empathy, and clarity in their interactions with patients, families, and colleagues. They learn to effectively communicate complex medical information in a clear and understandable manner, ensuring patient comprehension and engagement. Interdisciplinary communication is also emphasized to promote collaboration and continuity of care. Training programs incorporate role-play exercises, case studies, and simulated scenarios to practice effective communication strategies. By enhancing communication skills, healthcare professionals can build trust, foster therapeutic relationships, and improve patient satisfaction, ultimately leading to safer and more patient-centered care.
Session on Simulation-Based Learning for Nursing Education
Simulation-based learning has revolutionized nursing education by providing immersive and realistic experiences for students to develop their clinical skills. Through high-fidelity manikins, virtual reality, and computerized simulations, nursing students can practice complex procedures, critical thinking, and decision-making in a safe environment. Simulations offer opportunities to enhance teamwork, communication, and problem-solving skills. Students receive immediate feedback, allowing them to reflect on their actions and improve their performance. This experiential learning approach prepares nurses for real-life clinical situations, increasing their confidence and competence. Simulation-based learning bridges the gap between theory and practice, ensuring that nursing graduates are well-prepared to provide high-quality, patient-centered care in diverse healthcare settings.
Session on Ethical Issues in Nursing Education and Patient Care
Ethical issues in nursing education and patient care require careful consideration to uphold the highest standards of professionalism and patient well-being. Nursing education addresses ethical dilemmas by teaching students about ethical frameworks, confidentiality, informed consent, and the rights and autonomy of patients. Students learn to navigate issues such as end-of-life care, cultural and religious beliefs, and resource allocation. Ethical principles guide decision-making in patient care, ensuring respect, beneficence, and non-maleficence. Nursing programs foster critical thinking skills and ethical reasoning to help students analyze complex situations and make morally sound choices. By addressing ethical issues in education and practice, nurses are prepared to uphold ethical standards, advocate for patients, and provide compassionate and ethical care.
Session on Role of Nurses in Disaster Preparedness and Response
The role of nurses in disaster preparedness and response is critical for ensuring the health and safety of affected populations. Nurses are trained to provide immediate and comprehensive care during emergencies, such as natural disasters or disease outbreaks. They play key roles in triaging and treating patients, coordinating emergency response efforts, and providing emotional support to survivors. Nurses also contribute to disaster preparedness by participating in drills and training exercises, developing emergency response plans, and educating the community on disaster preparedness measures. Their expertise in assessing and managing healthcare needs in crisis situations makes them invaluable assets in disaster response, helping to save lives and alleviate suffering.
Session on Integrating Mental Health Education in Nursing Curriculum
Integrating mental health education in nursing curriculum is vital to equip future nurses with the knowledge and skills to address the growing mental health needs of patients. Nursing programs focus on teaching students about mental health disorders, assessment tools, therapeutic communication techniques, and evidence-based interventions. By integrating mental health education, students develop a holistic understanding of patient care, recognizing the importance of mental well-being in overall health. They learn to identify early signs of mental health issues, provide support, and promote mental health promotion strategies. Nursing curriculum ensures that nurses are prepared to address the complex mental health challenges faced by individuals and communities, enabling them to provide compassionate and effective care in a variety of healthcare settings.
Session on Promoting Wellness and Self-Care for Nurses
Promoting wellness and self-care for nurses is essential for maintaining their physical, mental, and emotional well-being. Nursing programs emphasize the importance of self-care practices and stress management techniques. Students learn about the impact of work-related stress, burnout, and compassion fatigue. They are taught strategies such as regular exercise, healthy eating, adequate sleep, and relaxation techniques to support their own well-being. Additionally, nursing programs foster a culture of support and encourage nurses to prioritize self-care through regular breaks, peer support, and access to counseling services. By promoting wellness and self-care, nursing education seeks to empower nurses to prioritize their own health, leading to increased job satisfaction, improved patient care, and long-term career sustainability.
Session on Innovations in Clinical Education and Experiential Learning
Innovations in clinical education and experiential learning have transformed the way healthcare professionals are trained. Traditional models have been augmented with technology-driven tools, such as virtual patient simulations and augmented reality applications, allowing students to practice clinical skills and decision-making in realistic scenarios. Interprofessional education initiatives have been implemented, promoting collaboration among different healthcare disciplines to improve patient outcomes. Furthermore, community-based learning experiences and global health rotations provide students with diverse exposure and cultural competence. These innovations in clinical education foster critical thinking, teamwork, and adaptability, preparing healthcare professionals to navigate complex healthcare environments and provide high-quality, patient-centered care.
Session on Addressing the Aging Population through Geriatric Nursing Education
Addressing the aging population through geriatric nursing education is crucial to meet the unique healthcare needs of older adults. Nursing programs incorporate specialized coursework and clinical experiences focused on gerontology. Students learn about age-related conditions, geriatric assessment, medication management, and strategies for promoting independence and quality of life in older adults. Geriatric nursing education also emphasizes person-centered care, cultural sensitivity, and communication skills specific to older adults. By equipping nurses with specialized knowledge and skills, geriatric nursing education ensures that older adults receive comprehensive, compassionate, and evidence-based care. This helps promote healthy aging, prevent complications, and improve the overall well-being of the aging population.
Session on Nursing Informatics and Healthcare Technology Integration
Nursing informatics and healthcare technology integration have revolutionized the way healthcare is delivered and managed. Nursing programs emphasize the importance of understanding electronic health records, data analytics, and healthcare information systems. Students learn to navigate and utilize technology for efficient and accurate documentation, medication administration, and care coordination. Additionally, nursing informatics education covers concepts such as interoperability, privacy, and security of health information. By integrating nursing informatics, nurses are equipped to leverage technology to improve patient outcomes, streamline workflows, and enhance communication among healthcare teams. The integration of healthcare technology and nursing informatics optimizes the delivery of safe, effective, and patient-centered care in today's digital healthcare landscape.
Session on Promoting Diversity and Inclusion in Nursing Education
Promoting diversity and inclusion in nursing education is crucial for creating a culturally competent and equitable healthcare workforce. Nursing programs prioritize recruiting and supporting students from diverse backgrounds, ensuring representation and inclusivity. Curricula incorporate content on cultural competency, social determinants of health, and addressing healthcare disparities. Inclusive teaching strategies and simulations with diverse patient populations enhance students' understanding and empathy. Nursing education also fosters a respectful and inclusive learning environment that values diverse perspectives and experiences. By promoting diversity and inclusion in nursing education, future nurses are prepared to deliver culturally sensitive care, advocate for marginalized communities, and contribute to reducing healthcare disparities.
Session on Patient-Centered Care and Patient Advocacy in Nursing
Patient-centered care and patient advocacy are foundational principles in nursing that prioritize the well-being and autonomy of patients. Nursing education emphasizes the importance of developing strong communication skills and fostering therapeutic relationships with patients. Students learn to actively involve patients in their care, respect their preferences, and address their unique needs. Patient advocacy is taught, empowering nurses to speak up for patients' rights, ensure informed consent, and navigate the healthcare system on their behalf. By promoting patient-centered care and advocacy, nursing education instills a commitment to compassionate and respectful care, empowering nurses to be strong advocates for their patients' well-being and ensuring their voices are heard in the healthcare process.
Research Excellence Awards
Expert Level (Scientific Service Achievement Award)
The award to the experts who have made outstanding contributions to advancing in Nursing. It is the most prestigious award of the whole conference and is tagged as scientific service Achievement award. The eligibility criteria for achieving this award is that one should have minimum of 20+ years of experience in the relative field in public or private sector. The receiver of this award should have a dedicated fascination and should take initiative in researching the recent trends and developments towards the related subjects. You can nominate deserving of the award through online.
Professional Level (The Research Contribution Award)
The Award for professional or academic research activity acquired in Nursing research field in the public or private sector for experts having research knowledge at 10+ years in the field of Nursing with most relevant accomplishments. Part-time research experience would be counted as pro-rata. It is calculated starting from the date when you obtained the (first) degree entitling you to embark on a doctorate (either in the country in which the degree was obtained or in the country in which the researcher is recruited), even if a doctorate was never started or envisaged. You can nominate deserving of the award through online.
Scholar Level (The Upcoming Researcher Award)
The conference offers Scholar Level Award for the upcoming scientists, researchers and experts having 10+ years research experience in the field of Nursing. Our conference would like to provide best platform to expand your network by sharing your research knowledge at stage. Presentation includes 25-30 minutes of oral talk on the scientific research topics based on the theme of the conference along with 5 minutes panel discussions. You can nominate deserving of the award through online.
Women Scientist (The Women of Science Award)
Our Conference provides a unique platform for women scientists for presenting latest research projects with an in-depth analysis. We cordially invite women scholars and scientists from Universities/ Industries to who have 10+ years of research experience to join the forum. We are happy to encourage our women scientist’s participants through research awards and provide assistance for women scholars in career development and research guidance through our collaborations. Women Scientist can nominate deserving of the award through online.
Outstanding speaker in GLOBAL NURSING EDUCATION 2024
This award is recognizing for individual who will present their projects, strategies, and schemes that have been implemented to improve long-term excellence in Nursing. You can nominate deserving of the award through online
Best Keynote Speaker in GLOBAL NURSING EDUCATION 2024
This award is recognizes for best Keynote speaker who will present their projects, strategies, and schemes that have been implemented to improve long-term excellence in Nursing. if you were confirmed as keynote presenter from the program manager, you can nominate someone deserving of the award through online
Best Poster Presentation in GLOBAL NURSING EDUCATION 2024
Student Poster Competition is organized at Conference, to encourage students and recent graduates to present their original research. All accepted abstracts will be presented at the poster sessions during the conference. Conference Series aims at setting a platform for all the budding scientists and researchers to present their real-time work and share their views and aspects related to the theme of the conference. You can nominate someone deserving of the award through online.
Outstanding Masters/Ph.D./Post Doctorate thesis work Presentation in GLOBAL NURSING EDUCATION 2024
This award is recognizing for Masters/Ph.D./Post Doctorate thesis work Presentation who will present their projects and thesis that have been implemented to improve long-term excellence in the field of Nursing. You can nominate deserving of the award through online. You can nominate someone deserving of the award through online.
Become an Exhibitor or Vendor!
The 27th Global Nursing Education, Healthcare and Patient Safety Conference is a fantastic opportunity for exhibitors and vendors to showcase their products and services to an engaged audience of healthcare professionals. Taking place on April 25-26, 2024 in Amsterdam, Netherlands, the conference will bring together experts from around the world to discuss the latest developments and trends in the healthcare industry. Exhibitors and vendors will have access to a large and diverse audience, with opportunities to network, build partnerships, and generate leads. Don't miss this chance to connect with key decision-makers and showcase your offerings!
Become a Sponsor!
Sponsoring the 27th Global Nursing Education, Healthcare and Patient Safety Conference in Amsterdam, Netherlands on April 25-26, 2024 is a great way to showcase your brand and support the healthcare industry. As a sponsor, you will have access to a diverse audience of healthcare professionals, with opportunities to showcase your products and services, build brand awareness, and develop partnerships. Your support will also help to advance the conversation around nursing education, healthcare, and patient safety. Don't miss this opportunity to connect with key decision-makers, promote your brand, and demonstrate your commitment to the healthcare industry.
Market Analysis
The market analysis for global nursing education, healthcare, and patient safety in 2023 reveals a transformative landscape. The demand for nursing education programs is on the rise, driven by the increasing importance placed on quality care and patient safety worldwide. The healthcare industry is undergoing significant technological advancements, with virtual simulations, artificial intelligence, and telehealth solutions revolutionizing nursing education and transforming patient outcomes.
In 2023, there is a growing focus on preventive care, personalized medicine, and population health management, necessitating a skilled and adaptable nursing workforce. The aging population and the global burden of chronic diseases further contribute to the demand for healthcare services.
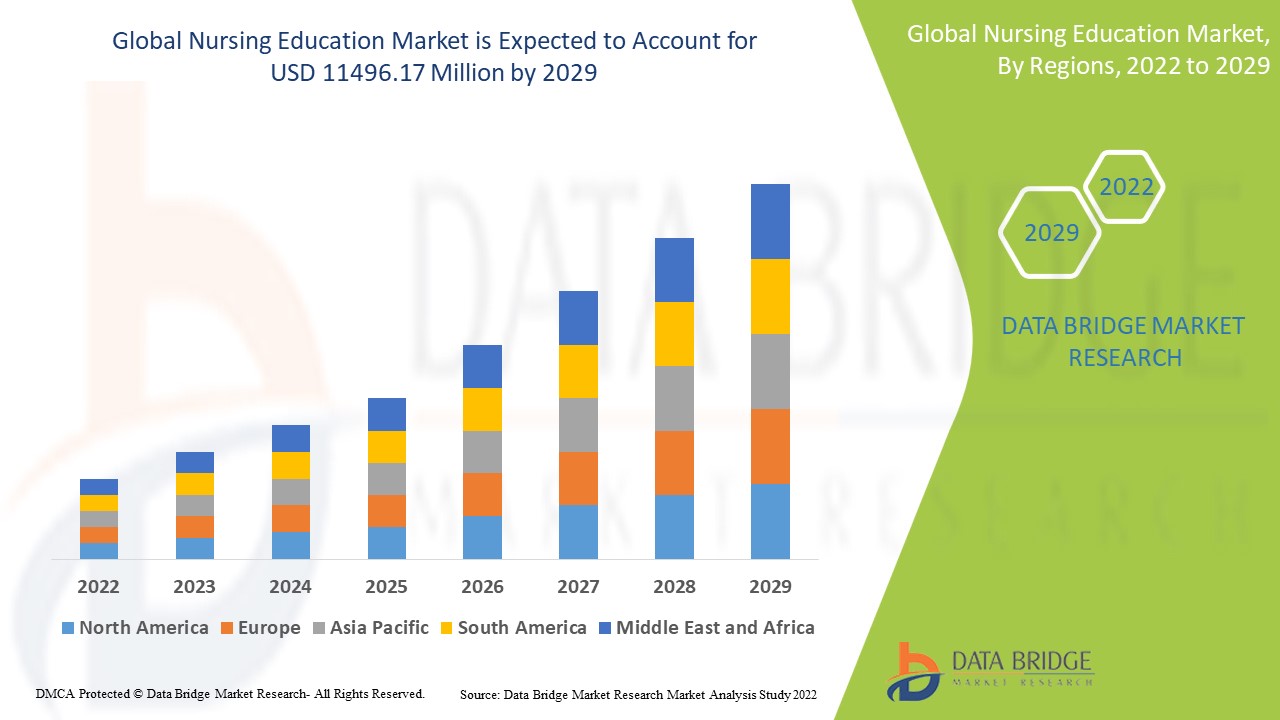
Market trends indicate the need for innovative educational approaches, such as online learning platforms and experiential training programs, to meet the evolving needs of nursing students. Collaborative partnerships between educational institutions, healthcare organizations, and technology providers are crucial for developing comprehensive solutions and driving industry growth.
To succeed in this dynamic market, stakeholders must prioritize continuous innovation, adapt to emerging technologies, and place a strong emphasis on patient-centered care and safety. The integration of advanced technologies and interdisciplinary collaboration will play a pivotal role in shaping the future of nursing education, healthcare, and patient safety in 2023 and beyond.
To Collaborate Scientific Professionals around the World
Conference Date April 25-26, 2024
For Sponsors & Exhibitors
Speaker Opportunity
Useful Links
Past Conference Report
Supported By
All accepted abstracts will be published in respective Conference Series International Journals.
Abstracts will be provided with Digital Object Identifier by



